Amy Bell kept falling – once, twice, sometimes three times a eek.
“I’d just sort of crumple to the floor,” says the 81-year-old Calgary woman. “I couldn’t tell you how many falls I’ve had.”
A fall last summer required seven stitches to close the gash on her forehead. Her adult children decided something had to be done.
Bell’s doctor referred her to GARP, the Geriatric Assessment and Rehabilitation Program in Calgary, which helps frail older adults regain their independence.
“They check out old people, see how they’re doing and get them fit enough to go back into everyday life,” explains Bell, who spent four weeks at the hospital working with a team consisting of a physician, nurse, pharmacist, physiotherapist and occupational therapist.
The GARP team looked at the number of medications she was on – eight – and the doctor told her, “You’re taking enough to knock a horse down.”
Twenty per cent of seniors die within the first year following a hip fracture, and 50 per cent never regain full mobility.
Falling is so common we’ve come to believe it’s just a part of getting old.
That’s a myth, says Judy Hughes, a fall prevention resource nurse in Calgary with Alberta Health Services.
“Falling is not a normal part of the aging process,” says Hughes. “And so many falls can be prevented.
“Falls are a result of underlying things. It’s the tip of the iceberg. You always want to drill down and find what made that person fall versus saying it’s because you are old. It could be a number of reasons.”
She gives the example of an 85-year-old who suddenly takes a tumble. If it’s assumed that his age is to blame – not, say, a bladder infection or pneumonia, both of which can cause confusion and dizziness – it’s missing an opportunity to address a perfectly treatable problem.
And, as Bell learned, overmedication is often a culprit.
People over 75 are at higher risk because they’re on more medications, says Hughes, explaining that as people get older, drugs affect them differently. The organs don’t process medication as quickly and efficiently, leading to higher amounts circulating in the bloodstream longer.
And the very medications often prescribed to help elders lower anxiety, elevate mood and help with sleep affect their brains and their balance, putting them at higher risk for falls, she says. Alcohol can compound the problem.
It helps to fill prescriptions at the same pharmacy. Telling the pharmacist about all the prescriptions, over-thecounter medications, vitamins and herbal remedies a person takes will help him or her spot drug interactions.
Beyond medication, lack of physical fitness plays a big role in falls. In her assessment with GARP, Bell discovered that very weak leg muscles played a role in her falls.
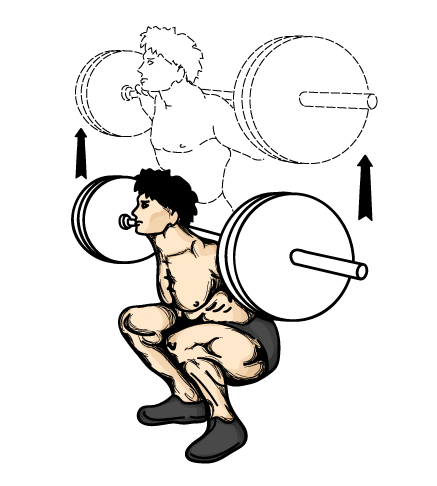
As people age, muscle mass shrinks, says Hughes. That’s why she and other experts advocate fall-prevention fitness programs to improve balance and build up elders’ thigh and core muscles. If they slip or trip, or a pet or grandchild gets underfoot, they can more easily “catch” themselves and stay upright.
Thirty minutes a day of exercise should include strength and balance exercises, such as lifting light weights, climbing stairs or doing tai chi. Walking, dancing and swimming build endurance. Stretching, yoga and tai chi improve flexibility. It’s important to exercise keeping in mind the health conditions you may have.
Dr. Debbie Rose, a kinesiologist and specialist in fall prevention from California State University, says an ideal assessment includes having an occupational therapist do a home visit.
The OT would evaluate safety issues – clearing clutter, getting rid of hazards such as throw rugs and installing grab bars in the bathroom – and how the older adult uses the space.
For example, an OT may move kitchen items so the senior doesn’t have to use a stepladder, but would still need to reach up and safely retrieve them.
“It’s not a question of making the home so easy to use that their physical activity declines,” says Rose.
Hughes dubs this the “Lazy Boy syndrome.”
“It’s the whole ‘I worked hard all my life and now I can sit back and not do anything. And guess what the kids bought us for Mother’s and Father’s Day? Chairs that lift you right up so you don’t even have to (use your muscles) to stand!’ “
Before she entered hospital, Bell had increasingly relied on her electric scooter. That made her even weaker, which made her more prone to falling. A vicious circle.
In the hospital, Bell had to use a walker to get to all her checkups and meals, initially always accompanied by a nurse.
As she became stronger through daily strengthening, stretching and balancing exercises, she graduated to using her walker unaccompanied.
The GARP team gradually weaned her off some medications, and lowered the dosage of others.
Widowed two years ago, Bell now needs less help dressing herself. Getting in and out of the bathtub is easier. She’s also lost weight and is sleeping better.
“A lot of things have been easier. I’d recommend the GARP program to anyone. It’s made a big difference for me,” she says.
Best of all, she hasn’t had a fall since September.
Hughes encourages more people to talk about falling.
“Seniors used to hide them, because they were afraid of being sent to a nursing home or long-term care facility. But falls aren’t normal. Check into it. You can do some things about it. We’re starting to normalize the topic of falls. You wouldn’t hide your high blood sugar, so why should you hide that you’ve fallen? Let’s get down to what caused it.”
CHRONIC DISEASES, DEMENTIA BIG PROBLEMS
In addition to falls, the major health problems in the elderly are chronic diseases such as heart disease, cancers, dementia and osteoporosis, says geriatrician Dr. David Hogan.
Acute problems such as influenza, infection and pneumonia also exact a toll on those over 75, as their bodies are less able to ward off viruses and bacteria.
More than 500,000 Canadians live with dementia, according to the Alzheimer Society, with those numbers expected to climb rapidly as the population ages.
Currently, there is no recommendation to routinely screen for dementia, says Hogan.
Unfortunately, he says, current tests for dementia aren’t that accurate, and even if dementia is identified early there are not a lot of interventions that have been shown to slow down the rate of progression.
© Copyright (c) The Montreal Gazette
